Phorest & Trees: Gobble Gobble it up
It was nice to see family at Thanksgiving again. Hope you enjoy these.
AANEM & NEUROMUSCULAR STUFF
- Below is the most prolonged CMAP I’ve seen in the context of carpal tunnel. Has anyone seen longer?
- Attached
is the Gold Coast criteria which may serve as a welcome alternative to the
El Escorial Criteria for diagnosing ALS. This was brought up at the AANEM
conference as well.
- Because
someone asked for it, I dug up the AANEM’s position paper on ethics in the
EMG lab. If you have not read it already, please take a look at the very practical
content within.
- The AAN put out a position
statement on Social Media: "We created this new position statement
to build a framework of how to apply commonly accepted ethical principles
-- beneficence, nonmaleficence, autonomy, and justice -- to a form of
communication that is rapidly developing and ever-changing, but at the
same time separate that very strictly from giving explicit advice on how
to utilize certain forms or platforms of social media, because that is
something very different,"
- COVID bad. Rehab
good.
- Benefits
of steroids without the side effects?
- Transcranial
current to treat peripheral neve pain? Ultrasound
FDA approved for Parkinson’s?
- A lot of so-called CIDP
is actually CMT
Musculoskeletal/PAIN/Rheum
- “Intraarticular
corticosteroid injections are not associated with increased risk of
progression compared to hyaluronic acid.” This study is in
contrast to other recent data and would definitely affect my practice if
true.
- I
had to read about Relapsing
Polychondritis. Amazing that I’m still learning about conditions that
I’ve never heard of. “Realizing the depths of your own ignorance” as per
Shenoy.
- Fascinating
that virtual reality incorporating CBT principles to engage pain patients,
self management, deep relaxation, attention shifting, healthy movement
visualization and other skills (EaseVRx)
offered >50%
reduction in chronic back pain patients Supercool images in the
attached article about DECT 3D reformats to look at glenoids for signs of
instability. (just look at the yummy pictures).
- With
regard to corticosteroid injections and rapidly
destructive hip disease(RDHD), several of the Bradford-Hill criteria
(evaluating observed causal relationship between an exposure and a
disease) are met, including
strength of association, biological gradient, experiment, and biologic
plausibility. Specifically, the association between hip corticosteroid
injection and RDHD was strong, with an adjusted odds ratio of 8.56. There
is evidence of a biological gradient (also termed dose-response curve) as
the risk of RDHD increased with the number of injections as well as the
dose. Removal of the exposure was also shown to alter the frequency of the
outcome (experiment) as the rate of RDHD (regardless of cause) was found
to decrease in our region as the number of corticosteroid injections
(specifically high-dose injections) was reduced.
- Important
for the residents: MRI
of the lumbar spine performed early after onset of LBP symptoms was
associated with a higher probability of surgery, greater prescription
opioid use, increased costs of care, and higher pain scores. Similarly, in
patients with LBP who did not have red flag symptoms, routine
imaging did not provide health benefits and suggested medical imaging
was often performed because of a clinician’s need for a diagnosis, to
identify an anatomical defect, to meet the expectations of patients, or
for financial incentives.
- My
initial Vitamin D level was 9. Maybe
I should be exercising…
- Rheumatoid
arthritis is preventable
- See
attached high powered oral steroids for acute radic. “Whether the
observed improvement in function (without concomitant improvement in pain)
merits use of oral steroids for patients with an acute radiculopathy is a
difficult decision and, ultimately, becomes a personal one that must be
weighed by individual patients and their physicians. In addition, pain may
limit function, so as pain decreases, function (ODI) may increase until
pain again limits functional capacity. This may explain the improved
function without measurable improvement in pain.”
- Exercise
decreases urinary toxicity in radiation treated prostate cancer
patients
- Surgical
treatment for AC joint dislocation of the shoulder does not appear to
be superior to conservative management in adults resulting in similar
quality of life, function, and return to previous activities after one
year. Surgical therapy increases the risk of hardware complications,
infection, and continued discomfort. 1 (Strength of Recommendation: B,
based on inconsistent or limited-quality patient-oriented evidence.)
- A
measured and broad perspective of stem
cells in the regenerative landscape.
- Don’t
have a colonoscopy
before your total knee replacement
- Keeping
risk factors in check helped people with diabetes stave off dementia. Compared
with controls, Type 2 diabetics had no significant excess dementia
risk with 5-7 risk factors on target (nonsmoking; guideline-recommended
levels of glycated hemoglobin, blood pressure, BMI, albuminuria, physical
activity, and diet). Similarly, differences in processing speed, executive
function, and brain volumes were progressively smaller for a higher number
of risk factors on target.
- The
burden
of chronic low back pain on society
- Perioperative
acetaminophen in patients undergoing rotator cuff repair in this prospective
randomized study improved overall satisfaction and reduced pills taken
compared to oxycodone only.
- On
DOXIMITY: footwear
effects on arch stiffness during running, exercise
increases anti-inflammatory gut microbes and endocannabinoids, Oxy
aint no better than APAP + codeine post-op
fracture;
- Housework
physical activity is positively associated with functional health among
community-dwelling older adults, independent of recreation and other
non-recreational PAs.
- Current
research indicates that torus fractures should be managed with a removable splint
supplied in A&E and worn for 3 weeks. There is no need for fracture
clinic follow-up or repeat radiological imaging once patients are given
adequate information at the time of diagnosis.
- THA
can lead to spatially different remodeling of the sacrum, possibly
affecting the development of contralateral Sacral Insufficiency Fractures.
- JAMA
RESTORE
trial found no difference
between PRP & saline for knee OA. FWIW, since I have no experience
with it, a friend opined “The PRP was only 1.4 x concentration, it is
basically like taking your plasma and injecting it directly back in.
Worthless study IMO”
TREES
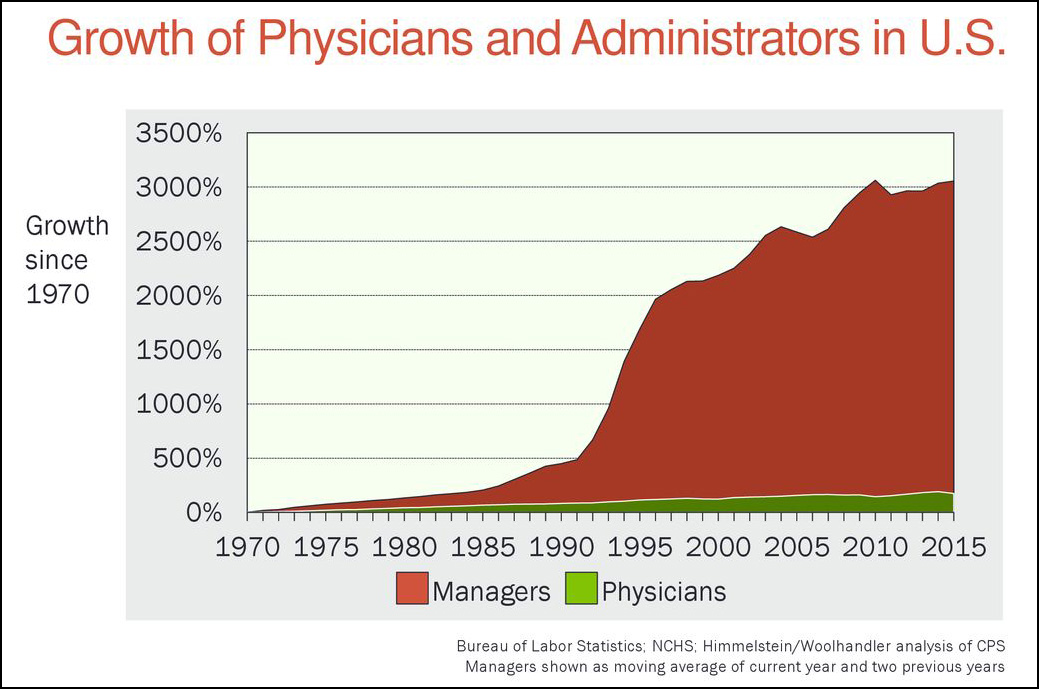
- I have LONG awaited a study showing the financial
and productivity drain of insurance companies. Here
it is!
- Space flight seems to cause the same biomarker
changes as brain
injury.
- Teaching COVID
& PMR
- Although it’s awesome that doctors are held to
one of the highest standards, maybe we are starting to be treated unfairly
with ageism. This
was a very well written discussion of the evolving issue.
- If not already a member, i encourage you consider
joining this facebook
physician group who have come together and actually addressed congress
to represent us.
- Market
data shows that more people are listening and they are listening
locally so that there are fewer and fewer megastars. The trends are in
favor of the little guy.
- AMA,
Other Physician Groups Strongly Oppose New VA Standards of Practice - U.S.
Medicine (usmedicine.com)
- Specific
pain conditions are associated with increased odds
of suicide attempts even after including key covariates.
- When
it comes to the booster decision, the federal
government has committed three cardinal sins. The White House
disrupted the process by making boosters seem a fait accompli when they
were not. The White House, the FDA, and the CDC focused the discussion on
the question of a broad approval of boosters for everyone over the age of
16, when that was unlikely to begin with. And the CDC’s Walensky chose not
only to overrule an expert panel, but to insist that she was doing no such
thing. By not recognizing the gravity of the action, she likely made it
easier for future CDC directors to erode ACIP’s authority. Following these
steps wouldn’t just result in better decision-making, it would have made
the process more transparent.
- First
Residency Program in Connecticut for Rehabilitation Physicians
Announced - UConn Today
- Learned
the word: Monopsony
in this
article which does a great job of outlining the shifting healthcare
ownership landscapes. Required reading to the end for business savvy
residents. For deeper dives, look
at the corrupting
influence of private equity groups and alternate
ways to maintain autonomy.
- A
nice description about Academic
mentoring
- FDA
is cracking down on fraudulent
e-stim
- Gene-editing
to protect 99% against Alzheimer’s or at least just drink a lot of coffee

.jpg)